In full transparency, the following is a press release from the Senate President’s office submitted to SOURCE media. (courtesy graphic)
***
[broadstreet zone=”59982″]
BOSTON – The Massachusetts State Senate on Tuesday, July 26, passed legislation to limit the use of step therapy, or ‘fail first’ protocols that too often direct patients to cheaper medications rather than those more suitable to treat their condition.
The bill, An Act relative to step therapy and patient safety, gives health care providers more leverage in determining the most effective treatment options for patients, saving patients expensive and painful regimens on medications they know to be ineffective or harmful.
This bill builds on similar legislation passed by the Senate in 2020.
“Health care decisions should be made by patients and their providers, not by insurance companies,” stated Senate President Karen E. Spilka (D-Ashland). “I’m proud that the Senate has taken the lead on limiting the use of step therapy as part of a wider strategy to shift the balance of health care back in the direction of the patient. I want to thank Senators Cyr, Friedman, and Rodrigues for continuing to refine and push for this legislation.”
[broadstreet zone=”59983″]
If passed, Massachusetts would join 28 other states in curbing unfair step therapy practices. The bill, An Act relative to step therapy and patient safety, now moves to the House of Representatives for consideration.
“Providing access to groundbreaking treatments that help improve the quality of life for those fighting cancer, debilitating diseases and a wide range of other medical conditions is a vitally important step we need to take, which is why the Senate acted again today to pass this critically important legislation,” said Senator Michael J. Rodrigues (D-Westport),Chair of the Senate Committee on Ways and Means. “I applaud Senate President Spilka for her continued leadership, Senator Cyr, our colleagues in the Senate and the coalition of patient advocates for their dedication, desire and hard work to help us move legislation forward that provides necessary guardrails around the use of step therapy, ensuring the safety and wellbeing of patients in need.”
“Patients with complicated illnesses should be receiving the medications that their doctors know they need—not repeatedly taking medications that they know to be ineffective just to help save on costs in the near-term,” said State Senator Julian Cyr (D-Truro),Senate Chair of the Joint Committee on Mental Health, Substance Abuse, and Recovery, who sponsored the legislation. “Waiting for treatment to fail first before utilizing a preferred medication often leads to worsening symptoms that cause complications and needless suffering for patients; it is a shortsighted practice that puts patients at unnecessary risk. Step therapy takes lower costs today in exchange for more harm, more hospitalizations, and more spending in the very near future. I am grateful to Senate President Karen Spilka for her leadership and vision and thank Senator Rodrigues and Senator Friedman for their partnership in advancing this critical legislation.”
[broadstreet zone=”59984″]
[broadstreet zone=”59946″]
“Reforming the insurance-mandated practice of step therapy is long-overdue,” said Senator Cindy F. Friedman (D-Arlington),Senate Chair of the Joint Committee on Health Care Financing. Step therapy or ‘fail first” protocols too often direct patients to cheaper medications rather than those more suitable to treat their condition. With this legislation, we will join over half the states in the country reforming these practices, putting the focus back on health care providers working with patients to offer the best treatment possible.”
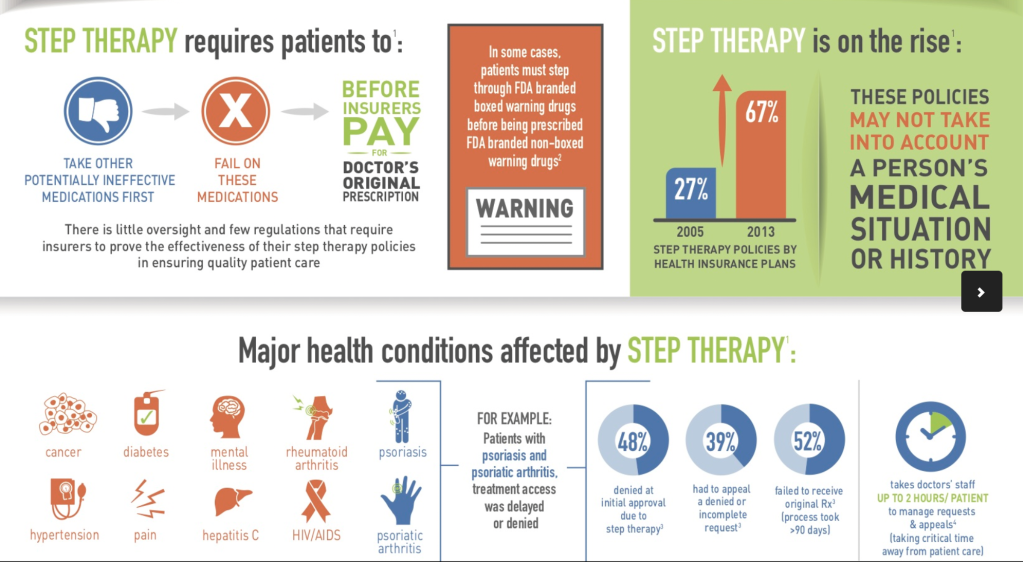
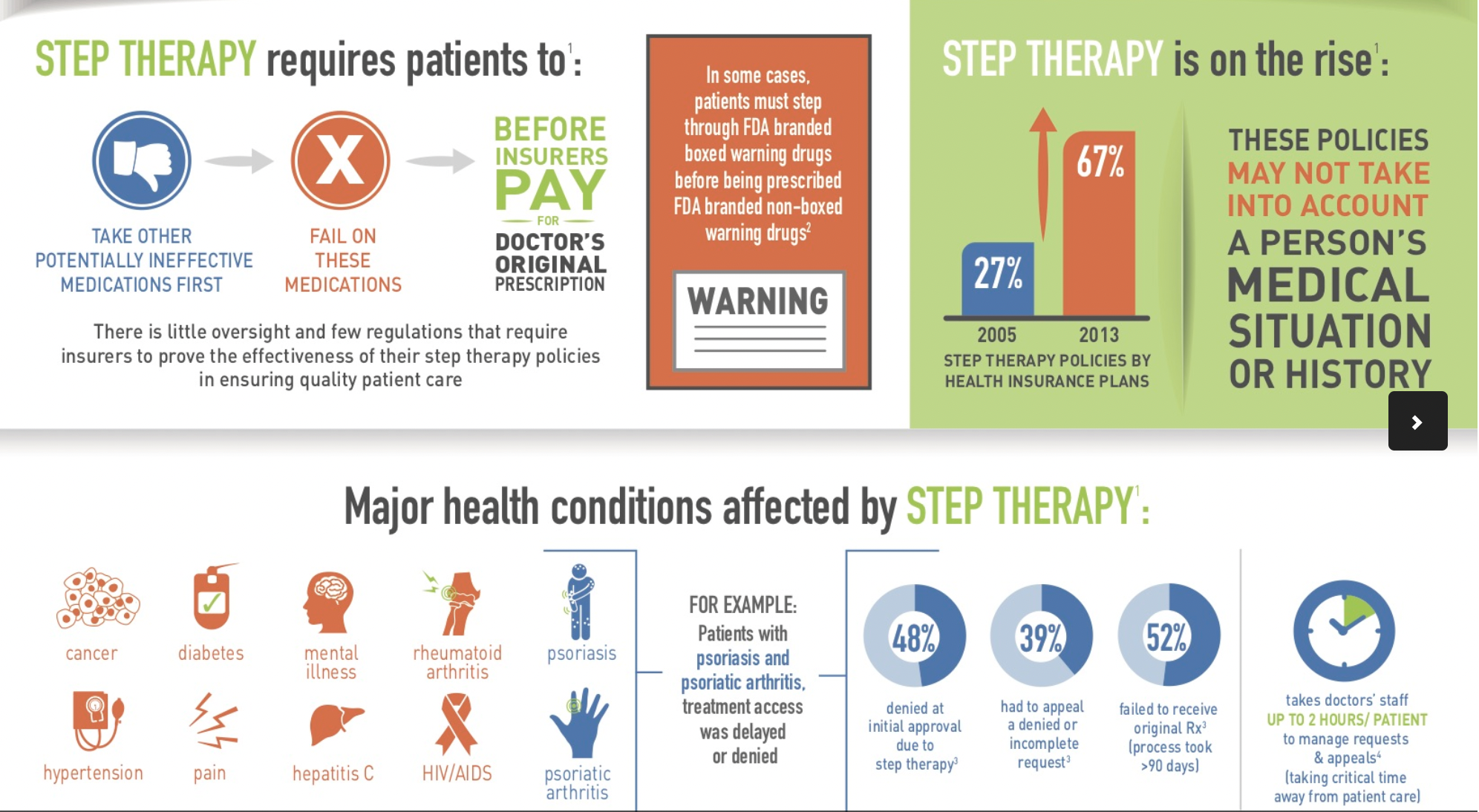
Step therapy serves as a cost-saving mechanism that can limit a patient’s ability to access the medication that is most suitable for treating their condition. Insurers that utilize step therapy protocols require medical providers to prescribe lower-cost medications to patients first, and only grant approval for alternative medications when the cheaper options have failed to improve a patient’s condition. In practice, this results in insurers effectively choosing medications for the patient, even in cases where their providers have recommended an alternative.
When patients change insurers, they are often forced to start at the beginning of the step therapy protocol again, which results in wasteful health care expenditures, lost time for patients, and potentially devastating health care impacts on the patient.
[broadstreet zone=”59947″]
Step therapy is not limited to specific diseases. It affects patients across the healthcare spectrum, with particularly dramatic impacts on the allergy and asthma, antipsychotic, arthritis, cancer, coronary artery, depression, diabetes, HIV/AIDS, multiple sclerosis, and Parkinson’s patient communities.
To address this, the bill establishes guardrails to protect patients in circumstances in which following step therapy protocols are counterproductive or harmful. The bill prohibits insurance providers from establishing a step therapy protocol that requires an insured individual to utilize a medication that is not likely to be clinically effective for the prescribed purpose. When establishing clinical criteria for step therapy protocols, the bill would ensure that insurance providers determine effectiveness through clinical review and take into account the needs of typical patient populations with similar diagnoses.
The bill provides patients who are subjected to step therapy sequences with an accessible exemption request process whenever coverage is restricted. The legislation enumerates specific timelines for insurers to review requests and grant exceptions, and in cases where interruptions in the patient’s medication schedule puts them at considerable risk, the turnaround time is faster.
[broadstreet zone=”53130″]
Under the bill, providers would accept or deny a request within 72 hours or within 24 hours if additional delay would significantly risk the insured individual’s health or well-being.
If an exception to step therapy is denied, the bill includes a process for the decision to be appealed.
Upon granting exemptions, MassHealth and private insurers would be required to provide coverage for the drug recommended by the patient’s provider.
To assist in future reforms, the bill would create a commission on step therapy protocols within MassHealth to study and assess the implementation of this bill and any future step therapy reforms.